The Anti-AI Stimulus: Why the "Boring" Money is Winning in 2026
If you spent the last month scrolling through LinkedIn or attending health tech mixers, you would be forgiven for thinking the only thing happening in healthcare right now is the deployment of autonomous AI agents. The hype cycle has fully pivoted from "AI as a tool" to "AI as a replacement," with endless pitch decks promising to automate everything from revenue cycle management to patient triage.
But while the venture world is looking at the stars, the federal government is pouring concrete.
The most significant news in health technology this month didn’t come from a product launch in the valley. It came from a bureaucratic filing deadline in Washington, D.C., where the Centers for Medicare & Medicaid Services (CMS) confirmed that states have overwhelmingly bought into the new wave of rural health funding.
We are witnessing the quiet launch of what I call the "Anti-AI Stimulus."
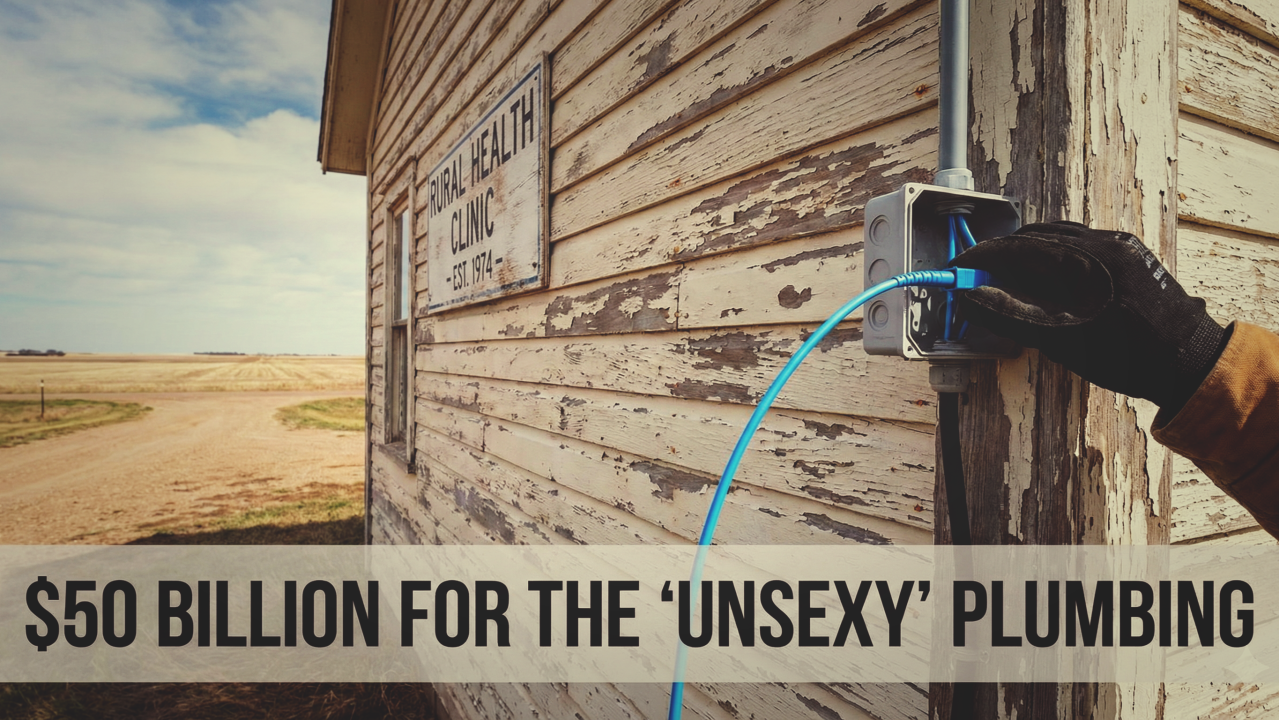
While the industry obsesses over Large Language Models (LLMs), the checkbooks for 2026 are opening for something far less sexy but far more critical: basic infrastructure. We are seeing a convergence of major funding streams, most notably the CMS AHEAD Model and the rapid expansion of Rural Emergency Hospital (REH) designations, that signal a massive shift in how care is delivered outside of major cities.
For the founders, investors, and strategists reading this: ignore this shift at your own peril. The smart money isn't chasing chatbots; it is chasing the plumbing that makes modern medicine possible.
The Policy Shift: From Volume to Value (Finally)
To understand where the money is going, you have to understand the problem the government is trying to solve. The rural hospital business model is broken. Recent data from The Chartis Group indicates that 50 percent of rural hospitals are operating in the red. They cannot survive on fee-for-service medicine because they simply do not have the volume.
The government’s response, through programs like the AHEAD Model, is to move states toward "global budgets."
In plain English, this means paying hospitals a fixed amount to keep a specific population healthy, rather than paying them for every MRI and surgery they perform. This is a radical reimagination of the financial incentives. When a hospital is paid a flat fee, keeping a patient out of the hospital becomes profitable.....but it also sounds like 'pop health', or 'at risk' models?!
This changes the technology wishlist overnight. If you are a hospital CEO under a global budget, you don't need a robot that does surgery faster. You need a remote monitoring platform that prevents the patient from needing surgery in the first place. You need data interoperability that actually works. You need the "boring" stuff.
The Conflict: A Turf War for Survival
There is a tension inherent in this funding that few are talking about. It is effectively a battle over the definition of "rural healthcare" and who controls the purse strings.
On one side, you have the Critical Access Hospitals (CAHs) and independent rural clinics. Their argument is straightforward: they are the physical lifelines in these communities. They view this capital as survival money intended to fix leaking roofs, update 15-year-old servers, and keep the emergency room lights on.
On the other side, you have the large academic medical centers in larger cities. Their argument is equally compelling: because rural facilities often lack specialized capabilities, the complex cases are transferred to the city. They rgue that they are the de facto safety net for the rural population and deserve a cut of the funding to maintain the "mothership" capacity. This isn’t just improved accounting; it is a fundamental strategic conflict. Is the goal to treat patients where they live, or to build better highways to the city?
The Technology Implications: The "Unsexy" Thesis
This is where the rubber meets the road for the health tech community. If you read the specific language in the Notice of Funding Opportunities related to these rural initiatives, the focus is on "sustainable access" and "technology-enabled solutions." If you are pitching a generative AI copilot that costs $100 per seat, you are likely barking up the wrong tree. The winners of these contracts will not be the companies selling "optimization." They will be the companies selling "foundation."
1. Cybersecurity is the Priority
We cannot ignore the reality that rural hospitals are currently the softest targets for ransomware. They are often running legacy software on deprecated operating systems, think Windows 7 or even XP running on MRI machines (a gross over exaggeration but you get the point), because they lack the IT budget to upgrade.
When a rural hospital gets hacked, patients get diverted, and people die. A significant portion of this new funding will go strictly toward cybersecurity hardening. It is not exciting. It will not make for a viral TechCrunch headline. But it is the prerequisite for everything else.
2. The Death of the "AI vs. Broadband" Debate
We love to talk about AI diagnostics in remote clinics, but those conversations are theoretical if the clinic has a shaky DSL connection that drops every time it rains.
The USDA’s ReConnect Program and similar initiatives are acknowledging that "digital health" is impossible without "digital access." Expect massive spending on "plumbing"; high-speed satellite links, secure data backbones, and reliable telehealth endpoints. You cannot deploy the future of medicine on 1990s infrastructure.
3. Workforce Extension, Not Replacement
The most viable "tech" play here is not replacing doctors, but extending the few we have left. Rural America is facing a massive shortage of specialists. We do not need AI to be the doctor; we need technology that allows one intensivist in a city to monitor patients across ten different rural ICUs simultaneously.
Tools that facilitate this "one-to-many" care model, like virtual nursing or e-ICU platforms, will find immediate product-market fit. The goal is leverage.
The Borderless Reality
As I wrote in The Borderless Healthcare Revolution, the concept of "borderless" care isn't limited to medical tourism or crossing international lines. The most difficult borders to cross are often the invisible ones within our own country: the county lines that separate a well-funded university hospital from a struggling rural clinic.
Technology has the power to erase those borders, but only if we invest in the right kind of technology.
The "hype" cycle tells us that the future is an AI agent that can diagnose a rare disease in seconds. The "reality" cycle, fueled by federal dollars and actual clinical need, suggests the future is a rural hospital that doesn't get hacked, has a stable internet connection, and can access a specialist without putting a patient in an ambulance for a three-hour drive in the snow.
If you are building for that future, 2026 is going to be a very good year.
#StayCrispy
-Dr. Matt